Category: Uncategorized
Maintain Your Muscle

Strength Training at Any Age
You’ve likely heard that exercise can help you live a longer, healthier life. When you hear the word ‘exercise,’ you might think of going for a run or hopping on a bicycle. Or maybe playing soccer with your kids or basketball with your friends after work. But these activities don’t include all the types of movements that are important for your health.
The examples above are endurance exercise. Also called cardiovascular exercise, activities like these increase your breathing and heart rate. They can keep your heart and lungs in good shape and help prevent many chronic diseases. But exercises to maintain flexibility, balance, and strength are also important.
Stretching gives you more freedom of movement and makes daily activities more comfortable. Balance practice helps prevent falls, which become a concern as you get older.
Strength training, also called resistance training or weight training, is particularly important. It brings many benefits. First, it makes your muscles stronger. That can help you keep up the activities you enjoy—at any stage of your life.
It’s not about getting big muscles, explains Dr. Wendy Kohrt, an aging expert at the University of Colorado. In fact, most people who do strength training don’t see much of a change in muscle size.
But at all stages of life, she says, “maintaining muscle mass and muscle function is really important for quality of life.”
Start Building Muscle Safely
Scroll through the images below for tips on getting started with resistance training.
Building Up Benefits
Building muscle can do more than make you stronger. Some types of strength training keep your bones healthy, too. Strength training can also improve the way your body processes food to help prevent diabetes and related diseases.
“And like endurance activity, regular strength training is associated with lower risk of cardiovascular disease and other chronic diseases,” says Dr. Joseph Ciccolo, an exercise researcher at Columbia University.
But the main benefit of strength training, as the name suggests, is that it makes your muscle cells stronger. “That benefit is unique to strength training,” says Dr. Roger Fielding, who studies the benefits of exercise at Tufts University.
Experts recommend that children and teens do muscle-strengthening activities at least three days a week. For adults, they encourage strength training for the major muscle groups on two or more days a week.
The benefits of strength training increase as you get older, says Fielding. Maintaining strength is essential for healthy aging.
“Loss of muscle with aging can limit people’s ability to function in their home environment and live independently,” Kohrt says. “Just being able to get up out of a chair or go up and down stairs requires a fair amount of muscle strength.”
In a recent study, Fielding and other researchers tested a three-month weight-lifting program in older adults who already had difficulty walking. At the end of the study, participants who lifted weights improved at tasks like repeatedly bending their knees. Such movements are essential for activities of daily living. In contrast, study participants who only stretched at home did not see similar improvements in strength.
“As we age, I think it’s even more important to consider incorporating some strength training into our physical activity routines,” says Fielding. “We can either slow down the progression of age-related muscle loss or prevent it.”
Getting Started
If you want to get started with strengthening exercises, what should you do? Strength training may seem intimidating if you’ve never tried it.
“People naturally learn to walk as part of growing up. But you don’t necessarily learn how to lift weights,” Ciccolo says.
If it’s feasible for you, booking a few sessions with a personal trainer is a good way to get started, says Kohrt. “That can get you introduced to the types of exercises you could do,” she explains.
There are also many low- or no-cost classes available. Look for them at local gyms, recreation centers, senior centers, and community centers.
Like with any new activity, to make strength training stick, “you have to find something that you really like to do,” says Fielding. “Some people will want to exercise in a group, in a community setting. Others will be happy doing all their exercises in their home, by themselves.”
If you’ve never lifted weights before, talk with your health care provider before you start any home-based strength training routine.
Whatever you choose to do, “start slowly and build up very gradually,” says Kohrt.
Source: NIH News in Health, March 2020
Resident’s Rights: What to Expect

When a loved one no longer is able to remain at home safely with supports it pays to have some basic knowledge when faced with the task of finding appropriate placement. Long-Term Care is a system unto itself with a language that most do not know if they have not had experience with either Skilled Nursing care or Assisted Livings facilities.
Take the time to explore options available for your loved one and take the time to personally visit facilities in the area that you would like your loved one to reside.
When you visit your facility options observe:
- The feeling of entering into the facility
- Smell or odors
- Volume of music, laughter, staff communications, other sounds
- Staff interactions with residents
- A meal when possible
Are:
- You greeted and welcomed by a staff
- Conversations with administration focused on financial rather than on resident care.
And visit during the weekend to observe staffing and the facility environment
The big Question is– are staff “Resident Centered”?
Types of Long -Term Care-
Skilled nursing care requires a skilled medical need for services to be authorized for insurance coverage. If the resident has Medicare it pays for the first 20 days and then the resident is required to private pay for the room and board for up to the next 100 days if there is no other payment source. For Medicare to cover, the individual must have a 3 day stay in the hospital. Medicare will not cover if the individual was admitted to the hospital for observation rather than treatment.
When an individual does not have a medical need for placement and is in need of long-term care services that is beyond assisted living care, options for payment may be long term care insurance, private pay or Medicaid.
The person Centered Care Plan in skilled Nursing Care or long term care guides the care that an individual has been assessed to need for their best quality of life.
Assisted Living level care is not a skilled level of care. According to Idaho Licensing and Certification “A Residential Assisted Living Facility is a facility or residence operated on either a profit or nonprofit basis for the purpose of providing necessary supervision, personal assistance, meals, and lodging to three or more adults”.
In an Assisted Living facility, the Negotiated Service Agreement guides the level of care required to meet the residents needs and increase or maintain their quality of life.
Residents and resident representative should have a voice in the development of these care plans.
Prior to signing an admission agreement—read the entire agreement and do not sign until you have read and understand what you are agreeing to. At a later time should you have questions or concerns it may be dependent upon what was in the admission agreement as to what rights you may have going forward. Keep a copy of the Admission Agreement that was signed upon admission.
Nationally staffing is at critical levels due to shortages. There has never been a more important time to be aware and involved in the long-term care of a loved one.
Know your rights. Every facility is required to post residents rights. When you have concerns or questions related to resident care contact your local Area Agency on Aging Long-Term Care Ombudsmen they are a great resource for information and resident advocacy.
Know who your advocates are and how to contact them- Ombudsmen are formally trained advocates that can help when family efforts aren’t enough.
Visit the ICOA website for additional information and services to help older Idahoan’s age with safety and dignity. www.aging.idaho.gov
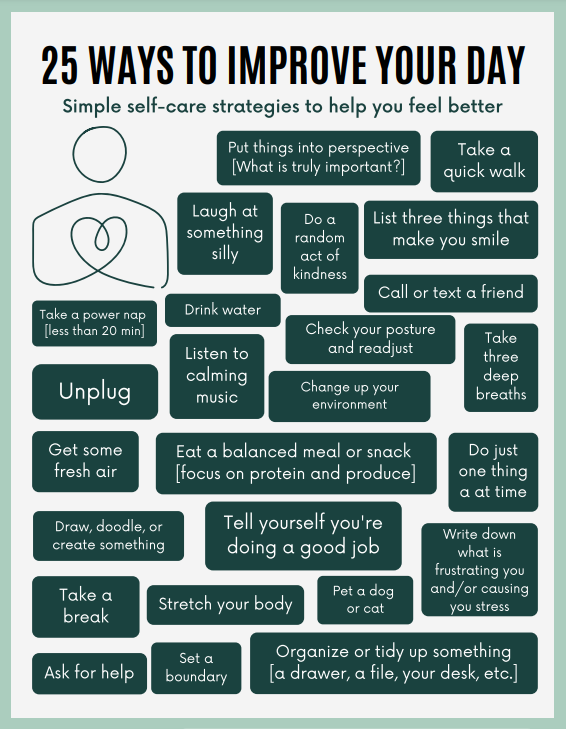
Prevent Burnout
25 Ways to Improve Your Day
Simple self-care strategies to help you feel better
- Put things into perspective [What is truly important?]
- Take a quick walk
- Laugh at something silly
- Do a random act of kindness
- List three things that make you smile
- Take a power nap [less than 20 min]
- Drink water
- Call or text a friend
- Check your posture and readjust
- Unplug
- Listen to calming music
- Change up your environment
- Take three deep breaths
- Get some fresh air
- Eat a balanced meal or snack [focus on protein and produce]
- Do just one thing at a time
- Draw, doodle, or create something
- Tell yourself you’re doing a good job
- Take a break
- Stretch your body
- Write down what is frustrating you and/or causing you stress
- Pet a dog or cat
- Ask for help
- Set a boundary
- Organize or tide up something [a drawer, a file, your desk, etc.]
Communication and Alzheimer’s

Alzheimer’s disease and other dementias gradually diminish a person’s ability to communicate. Communication with a person with Alzheimer’s requires patience, understanding and good listening skills. The strategies below can help both you and the person with dementia understand each other better.
- Changes in communication
- Communication in the early stage
- Communication in the middle stage
- Communication in the late stage
Additionally, the Idaho Commission on Aging website has Dementia Skills training that focuses on preparing and promoting communication and providing safe and comfortable care. See https://aging.idaho.gov/stay-educated/dementia-skills/.
Changes in the ability to communicate can vary and are based on the person and where he or she is in the disease process. Problems you can expect to see throughout the progression of the disease include:
- Difficulty finding the right words
- Using familiar words repeatedly
- Describing familiar objects rather than calling them by name
- Easily losing a train of thought
- Difficulty organizing words logically
- Reverting to speaking a native language
- Speaking less often
- Relying on gestures more than speaking
Communication in the early stage
In the early stage of Alzheimer’s disease, sometimes referred to as mild Alzheimer’s in a medical context, an individual is still able to participate in meaningful conversation and engage in social activities. However, he or she may repeat stories, feel overwhelmed by excessive stimulation, or have difficulty finding the right word. Tips for successful communication:
- Don’t make assumptions about a person’s ability to communicate because of an Alzheimer’s diagnosis. The disease affects each person differently.
- Don’t exclude the person with the disease from conversations.
- Speak directly to the person rather than to his or her caregiver or companion.
- Take time to listen to the person express his or her thoughts, feelings and needs.
- Give the person time to respond. Don’t interrupt unless help is requested.
- Ask what the person is still comfortable doing and what he or she may need help with.
- Discuss which method of communication is most comfortable. This could include face-to-face conversation, email or phone calls.
- It’s OK to laugh. Sometimes humor lightens the mood and makes communication easier.
- Don’t pull away; your honesty, friendship and support are important to the person.
Communication in the middle stage
The middle stage of Alzheimer’s, sometimes referred to as moderate Alzheimer’s, is typically the longest and can last for many years. As the disease progresses, the person will have greater difficulty communicating and will require more direct care. Tips for successful communication:
- Engage the person in one-on-one conversation in a quiet space that has minimal distractions.
- Speak slowly and clearly.
- Maintain eye contact. It shows you care about what he or she is saying.
- Give the person plenty of time to respond so he or she can think about what to say.
- Be patient and offer reassurance. It may encourage the person to explain his or her thoughts.
- Ask one question at a time.
- Ask yes or no questions. For example, “Would you like some coffee?” rather than “What would you like to drink?”
- Avoid criticizing or correcting. Instead, listen and try to find the meaning in what the person says. Repeat what was said to clarify.
- Avoid arguing. If the person says something you don’t agree with, let it be.
- Offer clear, step-by-step instructions for tasks. Lengthy requests may be overwhelming.
- Give visual cues. Demonstrate a task to encourage participation.
- Written notes can be helpful when spoken words seem confusing.
Communication in the late stage
The late stage of Alzheimer’s disease, sometimes referred to as severe Alzheimer’s, may last from several weeks to several years. As the disease advances, the person with Alzheimer’s may rely on nonverbal communication, such as facial expressions or vocal sounds. Around-the-clock care is usually required in this stage. Tips for successful communication:
- Approach the person from the front and identify yourself.
- Encourage nonverbal communication. If you don’t understand what the person is trying to say, ask him or her to point or gesture.
- Use touch, sights, sounds, smells, and tastes as a form of communication with the person.
- Consider the feelings behind words or sounds. Sometimes the emotions being expressed are more important than what’s being said.
- Treat the person with dignity and respect. Avoid talking down to the person or as if he or she isn’t there.
- It’s OK if you don’t know what to say; your presence and friendship are most important.
Please see Idaho Commission on Aging website https://aging.idaho.gov/caregiver/ for additional education and training, schedule of local events in our community and Area Agencies on Aging contact information.
Resource: alz.org/help-support/caregiving/daily-care/communications
Five Steps for Family Caregivers

Caring for a family member or a close friend is one of the most important roles you will ever play. It may start by simply running errands, driving them to their doctor appointment or shopping. Later, you may find yourself handling their medications, meals, finances, activities of daily living or other medical complexities. Therefore, it is important to know your loved one’s healthcare preferences with a plan in place before a crisis occurs. Here are five important steps to help you through this caregiving journey.
Step One: Start the conversation – “I just read an article about gathering all your important papers. Sometime can you show me where yours are and what you’d like us to do just in case?” Be open, express your love and concern, most importantly listen, and respect your loved one’s wishes regarding home, health, finances, and legal needs. Include other trusted family members to be a part of the process.
Step Two: Form Your Team – Go deep and wide and decide who is in charge. Team members do not have to live nearby or have lots of time available to be useful. Family or friends can work behind the scenes with meal planning/organizing, chores, bill paying, and assistive technology solutions.
Step Three: Make a Plan – Keep the plan simple and include immediate and future needs. There are several roles’ people can help with; an assertive advocate to communicate with medical professionals or insurance companies; if your loved one wants to move, assign someone to research locations and facilities. Someone else might offer to spend some weekends sorting through their personal belongings.
Step Four: Find Support – A variety of services are available to people aged 60 and over and their caregivers and older relative caregivers 55 or older. This support can be found through your local area on aging. The Idaho Commission on Aging website https://aging.idaho.gov/stay-educated/caregiver-skills/ provides an array of Caregiver Skills videos sponsored by AARP’s Home Alone Alliance. Additionally,
- Hire Help – housekeeping, meal preparation, laundry, shopping, bathing
- Secure Safety – Handrails, grab bars, night-lights, adjustable shower seats
- Stay organized – Caregiving apps such as Caring Village and Medisafe
Step Five: Care for yourself – Exercise, maintain a healthy diet, and sleep. Overall, be sure to take time for activities you enjoy.
Resource: https://www.aarp.org/caregiving/basics/info-2019/first-time-caregiver-tips.html?intcmp=AE-CAR-CRC-LL (AARP, Family Caregiving Guide)
Visit the ICOA Website for Caregiver information
Contact your local Area Agency on Aging for programs and services
For free education on healthy caregiving topics visit the Idaho Commission on Aging’s Caregiving Education webpage.
Emergency Preparedness for Older Adults
Follow these easy steps to make sure you’re protected.
Natural disasters, such as wildfires, floods, and blizzards, may force you to evacuate your home or shelter-in-place at short notice. It is important to know what to do in case of an emergency well before disaster strikes.
If you are an older adult living in the community, you may face some challenges during an emergency. For example, you may have mobility problems, or chronic health conditions, or you may not have any family or friends nearby to support you. Support services that are usually available, such as help from caregivers or in-home health care and meal delivery services, may be unavailable for a period of time. In addition, older adults may experience challenges that come with advanced age, such as hearing or vision problems or cognitive impairment, which may make it difficult to access, understand, and respond to emergency instructions.
You or the person you care for can be prepared for emergency situations by creating a plan, reviewing or practicing it regularly, and keeping an emergency supply kit.
Creating a Plan
The first step in preparing for an emergency is creating a plan. Work with your friends, family, and neighbors to develop a plan that will fit your needs.
- Choose a contact person who will check on you during a disaster, and decide how you will communicate with each other (for instance, by telephone, knocking on doors). Consider speaking with your neighbors about developing a check-in system together.
- Create a list of contact information for family members and friends. Leave a copy by your phone(s) and include one in your Emergency Supply Kit.
- Plan how you will leave and where you will go during an evacuation. If you are living in a retirement or assisted living community, learn what procedures are in place in case of emergencies. Keep a copy of exit routes and meeting places in an easy-to-reach place.
- Create a care plan and keep a copy in your Emergency Supply Kit. Try out the CDC’s easy-to-use care plan template.
- If you have medical, transportation, or other access needs during an emergency, consider signing up for SMART911, Code Red, or your local county registry, depending upon which service your area uses to helps first responders identify people who may need assistance right away.
Creating an Emergency Supply Kit
After an emergency, you may not have access to clean water or electricity. Make sure you are prepared with your own supply of food, water, and other items to last for at least 72 hours.
- Visit Ready.gov for a list of basic items to gather for your Disaster Supply Kit.
- Medical-Related Items:
- A 3-day supply of medicine, at a minimum. If medications need to be kept cold, have a cooler and ice packs available.
- ID band (full name, contact number for family member/caregiver, and allergies)
- Hearing aids and extra batteries
- Glasses and/or contacts and contact solution
- Medical supplies like syringes or extra batteries
- Information about medical devices such as wheelchairs, walkers, and oxygen including model numbers and vender.
- Documents (Keep physical copies in a waterproof bag and take photos of each document for backup):
- Contact information for family members, doctors, pharmacies and/or caregivers
- List of all medications, including the exact name of the medicine and the dosage, and contact information for pharmacy and doctor who prescribed medicine
- List of allergies to food or medicines
- Copies of medical insurance cards
- Copies of a photo ID
- Durable power of attorney and/or medical power of attorney documents, as appropriate.
Taking these steps will put you and/or your caregivers in a better position to deal with emergencies that may require you to evacuate or shelter in place. Contact your local Area Agency on Aging for information on senior services and resources in your area.
Bounce Back from Difficult Times

6 Ways to Nurture Your Resilience
Everyone goes through tough times in life. But many things can help you survive—and even thrive—during stressful periods. Nurturing your body, brain, and social connections can help you bounce back from stress. Use the six strategies below to get you started!
Develop healthy physical habits. Healthy eating, physical activity, and regular sleep can improve your physical and mental health.
Take time for yourself. Make taking care of yourself part of your daily routine. Take time to notice the good moments or do something that you enjoy, like reading a book or listening to music.
Look at problems from different angles. Think of challenging situations as growth opportunities. Try to see the positive side of things. Learn from your mistakes and don’t dwell on them.
Practice gratitude. Take time to note things to be thankful for each day.
Explore your beliefs about the meaning and purpose of life. Think about how to guide your life by the principles that are important to you.
Tap into your social connections and community. Surround yourself with positive, healthy people. Ask friends, family, or trusted members of your community for information or assistance when you need it. Look for cultural practices that you feel help in times of stress.
Source: https://newsinhealth.nih.gov/2022/04/nurture-your-resilience
Humor is Healthy

Laughing is both a physical and mental stress reliever. A good laugh can soothe tension, aid in relaxation, and release feel-good hormones to your brain. Laughter has also been shown to strengthen a person’s immune system and help relieve pain by encouraging the body to release its own natural painkillers. Best of all, out of everything you can do for stress management, laughter takes the least amount of effort and planning. Don’t let a day go by without a moment of laughter!

Smile!
Smile at those around you. Smiling is the beginning of laughter, and like laughter, it’s contagious. Plus, a smile releases hormones in your brain to lower stress.

Ask
Make humor part of the conversation. Ask friends, family members, and co-workers, “What is the funniest thing that happened to you today?”

Laugh at Yourself
Share your embarrassing moments. The best way to take yourself less seriously is to talk about the times when you took yourself too seriously.

‘Kid’ Around
Notice how children play and try to emulate them. They are the experts on being silly, taking life lightly, and laughing at ordinary things.
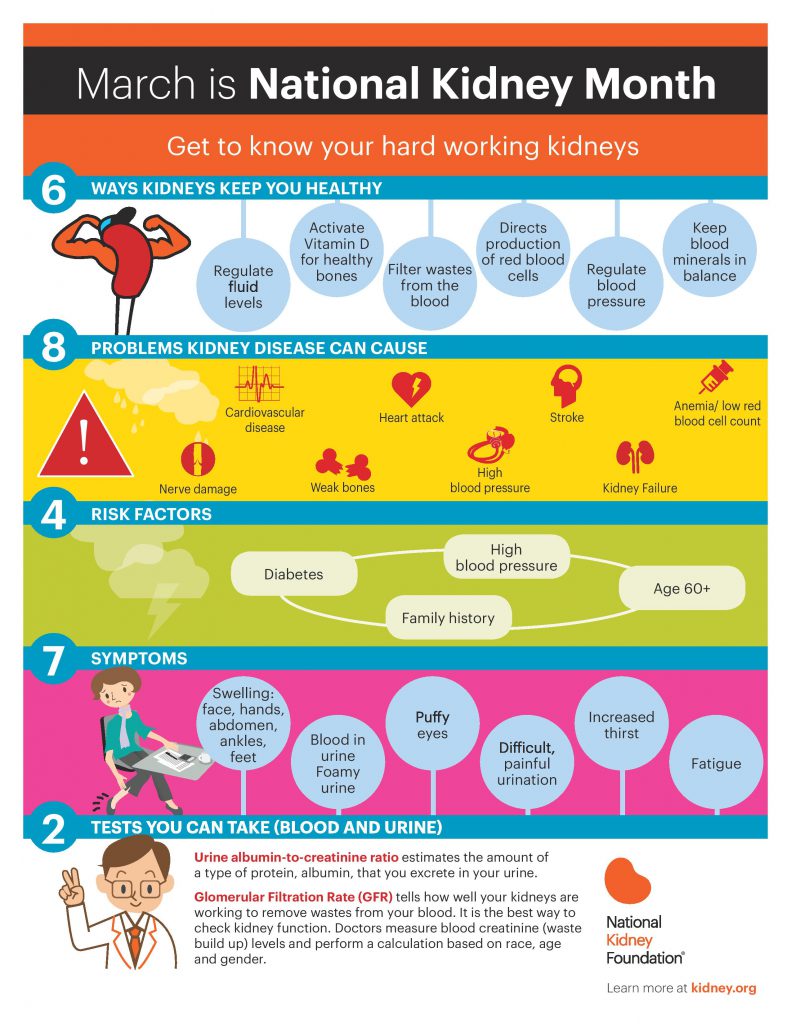
National Kidney Month

March is National Kidney Month! Did you know 100,000 people are currently waiting for a kidney transplant?! With so few organs available for transplantation, living donation is the best way we have to continue to save lives. Living donation takes place when a living person donates an organ (or part of an organ) for transplantation to another person.
Transplanting organs from a living donor has the following benefits:
- The quality of organs that are donated by living donors is usually better than organs from deceased donors. These organs last nearly twice as long.
- The waiting time for a patient needing a transplant can be significantly shorter.
- The procedure can be scheduled at a time that’s convenient for both the donor and recipient.
- The time between removing the organ (or part of the organ) and transplanting it in the recipient is less.
- There is a lower chance of rejection. Also, the organ recipient will need fewer and lower doses of anti-rejection medication.
Living Kidney Donation
Complete a confidential questionnaire to see if you qualify to be a living donor.
Crisis Coping Resources

ComPsych’s Guidance Resources®, the State of Idaho’s Employee Assistance Program provider, has shared the following resources to help cope with the anxiety and stress associated with global crisis and conflict.
Through the Employee Assistance Program, benefit eligible employees and their dependents may receive 1 to 5 visits per person, per issue, per plan year to confidential counseling services with no copayment required. Visit the Office of Group Insurance website to learn more.
Coping with Conflict Guide
- Dealing with the effects of social upheaval
- Coping with a traumatic event
- When anxiety becomes a problem
- Workplace resiliency in response to political discord
- Answering questions children have about tragedy
- Helping children cope with trauma
- Talking to a child during uncertain times
- Coping with grief
- Infographic: coping with stress and anxiety
- Infographic: when anxiety becomes a problem
Crisis Portal
- Coping with a traumatic event
- Coping emotionally after a disaster
- Talking to a child about a traumatic event
- What should I do when I am told to evacuate?
- Coping with grief
- Coping with a crisis or traumatic event
Coping During Uncertain Times Webinar Recording
People have a powerful need to understand and predict their environments in order to feel in control. When we are exposed to potential threats to our well-being, we naturally respond to this uncertainty with anxiety and fear. This training will address ways of effectively coping with uncertainty and will examine how to remain positive and functional, despite the risks of living in a changing world. Included will be practical tips for coping with uncertainty, re-establishing control, and tips for speaking to children about fear.
4 Mood and Energy Boosters
Your energy levels can be depleted by many factors. The external world is full of distractions, noise, sadness, and stress. It is valuable to remember that you, and only you, are responsible for your mood. Here are some helpful tips to keep your mood and energy levels in check so you can build them back up when they are depleted.

Music
A quick way to inject feelings of happiness and positivity is to include music. Music can provide an instant energy boost and has been used therapeutically in clinical settings for both pain management and emotional well-being. When you are feeling down or just need a dose of happiness, put on your favorite upbeat tunes, and groove your way to a better mood.

Laughter
It is true, laughter really can be the best medicine! Laughter has been shown to elevate mood, enhance immunity, and even prolong life. These benefits come from hearing laughter, having expectations of laughter or fun, and by the act of laughing itself.
Affirmations
Affirmations are phrases that you repeat to change, increase, or improve your state of mind. The power of affirmations is not in the words themselves, but the practice of visualizing a different reality. When you combine intentional actions with the refreshed mindset from your affirmations, you will find you can accomplish great things.

Good Deeds
When you do something nice for someone, it turns your focus away from yourself and your concerns and allows you to focus on helping somebody else feel good. Spreading kindness is the best way to spread happiness. Something as simple as a compliment, a kind word, or an act of generosity can start a positive domino effect of positive feelings.
Source: WELCOA’s COVID-19 Employee Education Toolkit: “Acknowledging and Lifting Your Mood and Energy Level“
Radon: Fact or Fiction?

Did you know radon is present in many Idaho homes? The Idaho Environmental Health Program within the Division of Public Health manages the Idaho Radon Program. Below is information to separate radon facts from fiction and help keep your family healthy.
FACT: All homes should be tested for radon.
Radon is a naturally-occurring radioactive gas that you cannot see, smell, or taste. It enters homes through gaps or cracks in the foundation. All homes, including new builds, existing homes, and those with and without basements, can have high levels of radon gas. With more people working from home due to the COVID-19 pandemic, the risk of radon exposure may be increased as more time is spent within the home.
Testing is easy and is the only way to know if you are being exposed to radon in your home. The Environmental Protection Agency (EPA) recommends testing your home every two years or after any remodeling.
You can order a FREE short-term test kit from www.radonidaho.org or call the Idaho Careline at 2-1-1 or 1-800-247-2435.
FICTION: Radon is not an issue where I live.
Two out of every five homes tested in Idaho have higher than the recommended levels for radon. In fact, high radon levels have been found in every county in the state. To learn more about radon test results and recommended actions, visit www.radonidaho.org. You can also view Idaho radon test results by zip code on an interactive map and order a FREE short-term test kit.
FICTION: Radon is not harmful to my health.
Long-term exposure to radon gas is known to cause lung cancer and is the leading cause of lung cancer in non-smokers. To learn more about the health effects of radon, visit the Environmental Protection Agency’s (EPA) Health Risk of Radon website at epa.gov/radon/health-risk-radon.
FACT: Winter is the best time to test a home for radon.
Radon levels can change by season and with the weather. The highest levels of radon are found during the winter months when homes get less fresh air. To learn more about radon testing and how to respond to a radon problem, visit www.radonidaho.org.
FACT: A radon problem can be solved!
Radon mitigation systems can effectively reduce the levels of radon in a home. The Idaho Radon Program recommends hiring a nationally-certified radon professional to fix your home. To locate a radon professional, visit www.radonidaho.org.
The Idaho Radon Program is offering a free two-hour interactive radon workshop that will explain what radon is, how it enters your home, and what you can do to help prevent excessive exposure and reduce your risk of lung cancer. To register, please visit www.radonidaho.org.
- January 18, 2022 at 1pm-3pm MT Virtual Online
- January 20, 2022 at 9am-11am MT City of Hailey, Council Chambers (*in-person masks required)
- January 25, 2022 at 9am-11am MT Virtual Online
- February 3, 2022 at 9am-11am MT Idaho Falls Building Department (*in-person masks required)
- February 17, 2022 at 1pm-3pm MT Virtual Online
If you have questions or need more information, contact the Idaho Radon Program at 1-800-445-8647 or radon@dhw.idaho.gov.
The 12 Ways to Wellness

The 12 Ways to Wellness
Sung to the tune of The 12 Days of Christmas
The first way to wellness said Health Matters to me,
Wash hands to be safe and healthy!
The second way to wellness said Health Matters to me,
Manage your stress, and wash hands to be safe and healthy!
The third way to wellness said Health Matters to me,
Drink water, manage your stress, and wash hands to be safe and healthy!
The fourth way to wellness said Health Matters to me,
Move your body daily, drink water, manage your stress, and wash hands to be safe and healthy!
The fifth way to wellness said Health Matters to me,
Prioritize your sleeeeeeeeeep, move your body daily, drink water, manage your stress, and wash hands to be safe and healthy!
The sixth way to wellness said Health Matters to me,
Eat fruits and veggies, prioritize your sleeeeeeeeeep, move your body daily, drink water, manage your stress, and wash hands to be safe and healthy!
The seventh way to wellness said Health Matters to me,
Understand your value, eat fruits and veggies, prioritize your sleeeeeeeeeep, move your body daily, drink water, manage your stress, and wash hands to be safe and healthy!
The eighth way to wellness said Health Matters to me,
Make time for self-care, understand your value, eat fruits and veggies, prioritize your sleeeeeeeeeep, move your body daily, drink water, manage your stress, and wash hands to be safe and healthy!
The ninth way to wellness said Health Matters to me,
Get vaccinated, make time for self-care, understand your value, eat fruits and veggies, prioritize your sleeeeeeeeeep, move your body daily, drink water, manage your stress, and wash hands to be safe and healthy!
The tenth way to wellness said Health Matters to me,
Plan a vacation, get vaccinated, make time for self-care, understand your value, eat fruits and veggies, prioritize your sleeeeeeeeeep, move your body daily, drink water, manage your stress, and wash hands to be safe and healthy!
The eleventh way to wellness said Health Matters to me,
Use good ergonomics, plan a vacation, get vaccinated, make time for self-care, understand your value, eat fruits and veggies, prioritize your sleeeeeeeeeep, move your body daily, drink water, manage your stress, and wash hands to be safe and healthy!
The twelfth way to wellness said Health Matters to me,
Build a social network, use good ergonomics, plan a vacation, get vaccinated, make time for self-care, understand your value, eat fruits and veggies, prioritize your sleeeeeeeeeep, move your body daily, drink water, manage your stress, and wash hands to be safe and healthy!
Small Steps, BIG Difference

November is National Diabetes Month!
Prediabetes is a serious health condition that puts you at an increased risk for developing type 2 diabetes. Prediabetes affects more than 1 in 3 U.S. adults—that’s 88 million people—but most people don’t know they have it.
The good news is that by making healthy lifestyle changes, it is possible to manage or reverse prediabetes and prevent it from turning into type 2 diabetes.
COULD YOU HAVE PREDIABETES?
Follow these tips to prevent/manage prediabetes:
01. Take small steps
Making changes to your lifestyle
and daily habits can be hard, but
you don’t have to change everything
at once. Start small.
02. Move more
Limit time spent sitting and try to
get at least 30 minutes of physical
activity 5 days a week. Start slowly by
breaking it up throughout the day.
03. Choose healthier foods and drinks more often
Pick foods that are high in fiber and low
in fat and sugar. Build a plate that
includes a balance of vegetables,
protein, and carbohydrates. Drink
water instead of sweetened drinks.
04. Lose weight, track it, keep it off
You may be able to prevent or delay
diabetes by losing 5 to 7 percent of
your starting weight.
05. Seek support from your doctor
People are more successful at
managing their prediabetes if they
have regular contact and support
from trusted health care professionals.
06. Stay up to date on vaccinations
The COVID-19 and flu vaccines are
important for people who may be more
likely to get very sick from COVID-19
or the flu, such as people with diabetes.
Resilience

Resilience is the ability to adapt and bounce back from stress, change, and challenge. Like a muscle, the more you exercise your resilience, the stronger it becomes. Being resilient doesn’t protect you from experiencing negative emotions, but it does help you embrace the opportunity to learn about yourself and prepare you for future challenges.
4 Ways to Revive Your Resilience

Get back to basics to boost your resilience.
Practicing positive lifestyle habits like good nutrition, sleep, hydration, and regular exercise can strengthen your body to adapt to stress and reduce the emotional impact.

Try to focus on what really matters to keep frustrations in perspective.
Focusing on the bigger picture can help you avoid blowing day-to-day annoyances like traffic and dirty laundry out of proportion.

Improve your mental health by leaning into positive social connections.
Work to keep relationships with friends, family, and co-workers strong so that you can be there for one another when times get tough.

Counteract the physical and mental side effects of stress by doing something that makes you feel good!
Laugh with a friend, move your body, or get to bed earlier. Doing just one thing that makes your body and mind feel a little better can help minimize the impact of stress.
Talk it Out
Talk to a mental health professional if you feel like you are unable to cope. The Employee Assistance Program [E.A.P.] provides confidential, short-term counseling services for benefit eligible employees and their dependents. You can call anytime to discuss marital, relationship or family problems; stress, anxiety and depression; grief and loss, job pressures and substance abuse.
 Official Government Website
Official Government Website